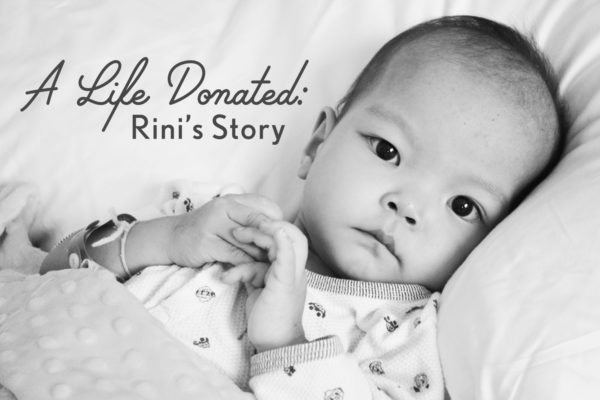
Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
From November 11, 2016
This day, three years ago, was the saddest of my life. Rini’s arrhythmias were continually worsening, clots were becoming more and more problematic, and I began to psychologically crack.

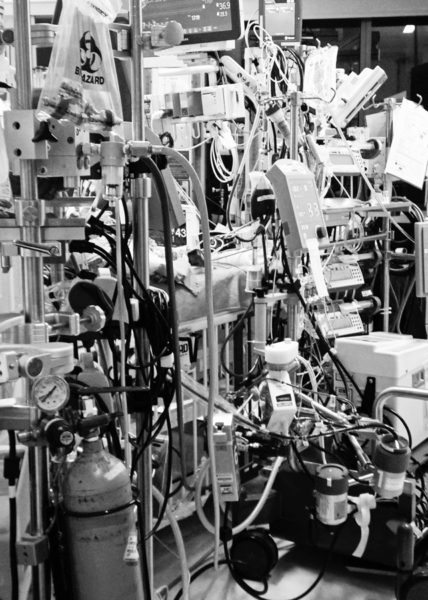
During rounds, the ECMO perfusionist was giving her report and she told the team that a clot had formed right where the ECMO cannula entered her artery. I remember being startled, and my eyes darting from one member of the group to the other trying to ascertain how concerned I should be by their expressions. But as always, their expressions remained unchanged.
At first I tried to comfort myself with that, but I knew better. I felt sick to my stomach and my ears began to ring. When they asked me if I had any questions, I said, “No.” I was in denial, but ultimately I couldn’t push it down any more. I pulled one of the transplant cardiologists aside and asked, “Should I be worried about that clot?” And she replied, “We are.” I asked what they were going to do about it, and she explained that there was nothing they could do about it at that point without putting Rini at extreme risk. Clamping the circuit and removing the cannula from her neck in an effort to reach the clot could inadvertently dislodge it and send it into her body, not to mention the amount of time she would be without blood flow.
The consequence of the clot dislodging into her body – a stroke – would not only mean possible death, but even if it didn’t kill her it would mean she would have to be removed from the transplant list. She went on to say that the risk of intervening was greater at that point than the risk of doing nothing. If the clot continued to grow, then their hands would be forced.

From my journal:
“It got to the point where I had to leave the room for several hours because watching yet another ECMO technician enter the room and look at the lines, sigh, discuss, sigh and on and on just became too much.”
I drove to a local grocery store, and as I walked down the aisle I felt completely detached from the world around me. I had tunnel vision, all sound seemed muffled and distant and I couldn’t feel my footsteps. I felt like I was floating.
When I returned to the hospital, I was walking down the long, white corridor on the 7th floor that connects the original hospital building to the new tower. There was a father on the floor, 40 feet or so from the entrance of the Pediatric Cancer Care Unit, curled up in the fetal position and sobbing. I could feel my own pain and desperation welling up within me, my need for control in a furious battle with my intellectual understanding that I had none.
I stopped in front of one of the multiple floor to ceiling windows that overlooked the parking lot. And at that moment, for just a moment, I wondered if God would forgive me if I threw myself through the window so that my baby could receive my heart. Surely He would understand a mother’s love, I told myself. Would my husband forgive me? What about my other five children? I couldn’t leave them without their mother. I’m not even a compatible blood type or size for what Rini needed. But I couldn’t just do nothing and let her die. Please God, I cried out, help me!
And like that father, I sank to the floor and cried for my child.
I had noticed a phrase being written many times over in the comments of people’s Facebook and blog posts…
“God has big plans for your child!”
I saw this being written in celebration of children who had survived accidents, surgeries, and illnesses. It always took me back to the idea that our society seems to hold that “life equals winning and death equals losing.” Surely God has big plans for all of us, regardless of how long we are on this Earth. In fairness, many people have no idea how to console a grieving parent, and no parent wants to hear someone say that their child’s death was meant to be or that it was God’s plan for their child to die. Someday I trust I will understand.
As a parent whose child was on the verge of death, it pained me to my core that the celebration of a child was so often attached to their surviving a battle. I watched as friends were preparing to say goodbye to their infants and children, only to have friends and family press them to not give up and to keep holding out for a miracle.
Why is the miracle recognized only in survival? The miracle is all around us. It is life. Not necessarily long life, just life. Rini is here with us, she survived that great trial. But her transplant is not a cure. The average graft survival for a pediatric heart transplant is 9-12 years. At ten years after transplant, 50% of children have passed away and others have already undergone re-transplant, which has been shown to have poorer outcomes than primary transplantation.
If Rini does not survive beyond that, does that mean her life wasn’t miraculous?
Exactly how long does someone need to be alive in this world before they are considered a miracle, and before the world sees their life as part of God’s great plan?
I didn’t want Rini or any child to be forgotten. I didn’t want anyone doubting God’s love or His miracles if she did not survive. So I made a promise to my daughter that even through death, her life would matter in a big way. And not just her life, but those of all of the children fighting for their lives and those children that had been lost.
God has big plans for all of our children, and I think that it is often up to those of us who remain to find meaning in our losses and bring those plans to fruition.
From November 12, 2016:
From my journal:
“The past two days have been the worst that I’ve experienced emotionally. By last night I was a wreck… shaking, crying, losing my voice. I was feeling like a heart would never come, feeling guilty for wanting one to come, grieving for my child, feeling ugly and awful for some of the thoughts and feelings I was having.”
On the afternoon of November 12, 2013 at approximately 2pm, I sat in the chair by Rini’s window to knit. Rini’s heartbeat had been steadily weakening and she was suffering from severe arrhythmias (the attached EKG was from that day). Eric and I had been receiving phone calls over the previous few days from our home hospital in Oregon… our surgeon, Child Life specialist and the director of the hospital’s hospice program. I knew that Seattle’s two transplant surgeons had been updating our home team daily, and with the information gleaned from conversations I’ve had over the past three years, I now see why those phone calls had been coming in. They understood where Rini was medically. She was very close to death, much closer than Eric and I understood.
I looked outside at the beautiful blue sky punctuated with bright white clouds, with rays of sunlight streaming down in between. I felt completely at peace. Warm, calm, and at peace. I had never experienced such a perfect peace prior or since. I said to myself, “I am ready to let Rini go, God. If she needs to go, if it is her time, I accept that. I will grieve mightily, but I give this to you because I can’t carry it. I will honor her and give purpose to her life, however short.”
The peaceful feeling continued as I knit. The ECMO Fellow came in and asked about my knitting. It turns out that he is a knitter, and I mentioned that perhaps we should begin an evening knitting club and what a hoot that would be! The room fell silent. In my peripheral vision to my right I noticed a figure, and I turned and saw that it was Dr. McMullen, one of the transplant surgeons. The reason for his presence in Rini’s room did not enter my mind. I just looked at him and said, “Hi! We were just talking about starting a knitting club! Would you like to join?” He smiled and said that he’d like to talk with me, and I offered him a seat.
“There is a heart, and it is Rini’s if she wants it.”
I felt completely and utterly calm. I looked around and everyone was looking at us. I sat in stunned silence as he talked about what was to come. He explained that there were some concerns with the donor’s heart (I would learn later that he was referring to its size and ischemic time, two issues that would cause serious problems during recovery), but that otherwise it looked very good. We were given the choice to turn it down, but I said, “We have to take it.” At the time of our conversation, the heart had not been seen inside the donor’s body yet, but it had been looked at via echocardiogram. There was the chance that it would be in worse shape than they thought and that they would not be able to use it for Rini, but we knew we would just take that as it came.
I signed the consent forms and our ECMO perfusionist took a few photos of Dr. McMullen and me together for Rini’s memory book.


From my journal:
“I then went out to the hallway and called Eric. He burst into tears and I went into business mode and began arranging childcare, canceling appointments, and the like.”
I called my parents, who reacted in stunned silence, as well as several close friends. And then I made a very important phone call to a woman I counted as one of my closest friends although we had never met nor spoken on the phone. Her son was on the heart transplant list on the East coast and many months before Rini had even been adopted, she had promised me that she would call me when her son received his heart. We never could have known that I would be making the call to her first. Her beautiful son received his new heart just a few weeks after Rini and is doing beautifully.
I went back to the room and a phone call came through, and it was Dr. Carlson, our kids’ cardiologist. She sounded so sad, and asked me how I was doing. I told her the news that the call for a heart had come just a little while earlier. Oh her voice! She sucked in her breath and she was so relieved. Later I learned that she had received word that morning that Rini’s was doing very poorly and not expected to live more than a few more days.
From my journal:
“We do not know where the donor is, and they cannot tell us. All we know is that the call came in from UNOS a few hours ago and that the dear child’s family has consented to all viable organs being donated, so transplant surgeons from around the country will be arriving at the donor’s hospital to receive lungs, kidney, liver, heart, and other tissues to take back to children and adults waiting. UNOS is still in the process of allocating all of the organs. This gift is amazing, indescribable, intensely life-affirming. Rini’s heart may be coming from as far as 2,000 miles away. Oh how I already feel connected to a family we have never met, a family who is devastated, processing their loss, and during that time has been able to think of others and of how their loss could be turned into something filled with love.”
I then spoke with one of the transplant coordinators who told me that the heart should arrive around 9pm (it’s arrival was delayed and it arrived at half past midnight), and she would be the one to take it into the OR and hand it off to the waiting transplant surgical team.
The operation was expected to take around 5 hours although, because of complications, Rini spent a total of 12 hours in the OR. It was explained that Rini’s transplant was considered high risk because of her pulmonary artery and lung issues plus her still tenuous nutritional status.
By that point, it was around 5pm and Eric was on his way to Seattle, and my parents were preparing to fly up from Los Angeles. Preparations for surgery were in the early stages in Rini’s room, and the weight of the emotional conflict within me was overwhelming.


How could I not be thinking of the donor and donor family and be mindful of their pain? Celebrating did not seem right, but neither did denying the joy inherent in the hope filled gift that was being offered. The word bittersweet was most apt for me during that time. Respectful, sacred, bittersweet celebration.
At that point in the day, Rini’s donor was still on life support at a hospital located (we would later learn) over 2,000 miles away. The child would not be removed from support until all of the various transplant surgeons had arrived from around the United States. There was a family still gathered around their child’s bed, perhaps taking hand and footprints, cutting a lock of hair, saying their goodbyes.
The heart was not Rini’s yet. The heart would be a gift, the most generous and selfless of gifts. Those hours leading up to the heart’s arrival were somber and holy to us. I prayed and prayed for the donor and family, and the parallels to adoption were stunningly apparent.
Eric and I have reflected upon that time and he said, “It was the most difficult time for me. I felt so torn. As a father, I felt like I had to pray for my daughter to receive a heart. But as a human being, I couldn’t pray for it since its arrival meant that another child had died.”
The doctor who was part of the palliative assistance team assigned to us in the CICU came and took me to the Quiet Room, where I cried and cried. She cried, too. She walked me through the process of determining brain death, of how a potential donor’s family is approached regarding the possibility of organ donation, how the families are treated with dignity and respect. And she told me that for those families, choosing to donate is a way for them to honor the child they have lost.
I was also so thankful to have had the counsel of a friend who both received an organ herself and donated her toddler’s when he died.
Eric arrived around 7pm, and by 8:30 the pre-op preparations were in full swing in Rini’s room. At almost 9:30, Rini was taken to the OR. It’s an awesome sight to see when a child on ECMO is being transported and on the way to hope and a future. We were permitted to accompany her to the last hallway before the OR, and there we kissed her and said our goodbyes.
After our child and her team were out of sight, we talked about the weight we felt lifted. Since the moment we chose to bring her into our family, we had fought for her. We fought for her adoption, fought for her care, and had brought her as far as we could in order to give her an opportunity to experience life, love, and family. Another family was now assisting us in that. And of course, God was there all along.
And together, Eric and I walked back to the CICU.
……..


























You have so touched my heart with your writing. xoxoxox Bonny in New Mexico.
Thank you so much for reading, Bonny!